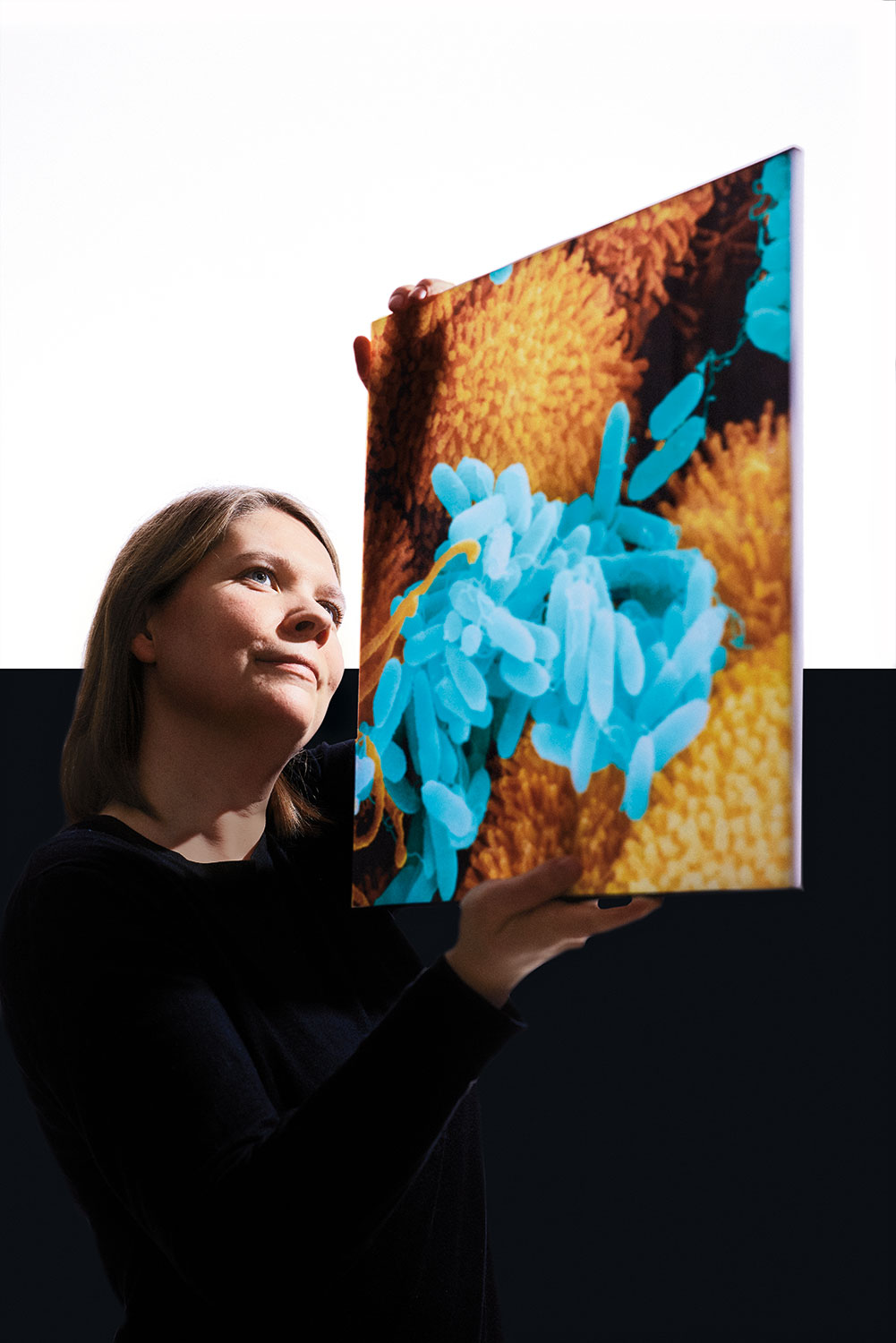
In addition to the use of the phages themselves, Loh and her team are also researching therapeutic uses for individual phage proteins. She explains: “A phage is made up of DNA inside a protein envelope. It also produces further proteins that can kill off bacteria. To destroy the bacteria, we use certain phage proteins that poke holes in the cell wall and cell membrane.” Loh likens an individual bacterium to a water balloon full of water, which is then pierced with ultra-thin needles: “At some point, it bursts.” The advantage of this method is that antibacterial proteins are not limited to highly specific strains of bacteria, instead having broader effects. “But simplifying the drug approval process is much more important,” Loh says. This is because unlike viruses, the therapeutic proteins can be produced as what are known as biologics. They could be used like chemical antibiotics. The issue, Loh says, is finding suitable proteins: “So, I look closely at every single phage and identify all the genes that could be of interest. Then I produce the proteins separately in bacteria and test them.”
But although phage research is currently gaining momentum, it will still likely be some time before the first preparations hit the market. Until then, it is even more important to curb the spread of dangerous pathogens and minimize the number of infections, especially in hospitals and nursing homes. To that end, a team of researchers at the Fraunhofer Institute for Manufacturing Engineering and Automation IPA in Stuttgart had a simple yet highly effective idea that has already been tested successfully at two hospitals: antimicrobial wall paint that reliably kills bacteria and viruses. Dr. Christina Bauder, head of the Applied Coating Technology team, explains: “We added photocatalytically active pigments to the paint. They are activated by natural light or artificial indoor light, at which point they form radicals that react with the surfaces of the germs and destroy them.” The pathogens do not even need to come into direct contact with the wall surface, either; it is sufficient if the air circulation brings them into the immediate vicinity. “The nice thing about our method is that the chemical reaction continues indefinitely. The photocatalyst isn’t used up,” Bauder points out. That is because it uses oxygen and water from the air inside the room to produce radicals that are harmless to humans. And that means the paint remains effective permanently, unlike other antimicrobial coatings that gradually release substances to kill germs. “Once those substances are used up, the protection wanes. That can’t happen with our method. Even in darkness, our photocatalyst has residual activity lasting at least 24 hours,” Bauder says. The results of the field tests conducted at the Oberschwabenklinik medical center in Ravensburg and at Kantonsspital Graubünden hospital in the Swiss city of Chur are impressive: The paint was highly effective, and swabs taken by researchers showed that the walls were nearly germ-free.
Even with all these approaches and potential solutions, the antibiotic crisis is still very dangerous, as there is a particularly acute issue: Antibiotics are not lucrative. Prices are low, development costs high. “We should actually be able to do more about this creeping pandemic, as Lothar Wieler, former president of the Robert Koch Institute, once called it,” says Dr. Dorothee Winterberg from Fraunhofer ITEM. There are many research initiatives, she says, but unfortunately not enough money. Winterberg sighs: “It’s enough to drive you crazy at times.” Prof. Till Schäberle from Fraunhofer IME agrees. “The market isn’t going to solve this on its own. The state needs to step in,” he adds. He has high hopes for large global funding initiatives like CARB-X, whose supporters include the Bill & Melinda Gates Foundation, the U.S. and Canadian governments and the German Federal Ministry of Education and Research (BMBF). Schäberle is firm in his prediction: “It is necessary, so we will see action on this front.”